ABOUT BHCPF
The Basic Health Care Provision Fund (BHCPF) was established under section 11 of the National Health Act as a catalytic funding to improve access to primary health care. The BHCPF serves to fund aBasic Minimum Package of Health Services (BMPHS), increase the fiscal space for health, strengthen the national health system particularly at primary health care (PHC) level by making provision for routine daily operation cost of PHCs, and ensure access to health care for all, particularly the poor, thus contributing to overall national productivity. The BHCPF is derived from (a) an annual grant from the Federal Government of Nigeria (FGoN) of not less than one percent (1%) of the Consolidated Revenue Fund (CRF); (b) grants by international donor partners; (c) funds from any other source, inclusive of the private sector. The BHCPF is implemented by 3 gateways namely, the National Primary Health Care Development Agency (NPHCDA) gateway which provides operational cost(Decentralized Facility Financing – DFF)and Human Resource for Health (HRH)for PHCs through the State Primary Health Care Board (SPHCB), the National Health Insurance Scheme (NHIS) gateway which insures the most vulnerable Nigerians to access the BMPHS through the State Social Health Insurance Agencies(SSHIA) and the National Emergency Medical Treatment (NEMT) gateway which is expected to cater for emergency ambulance services.
OVERVIEW OF THE NPHCDA GATEWAY
The NPHCDA is responsible for the implementation of the NPHCDA Gateway through the State Primary Health Care Boards/Agencies (SPHCB/A) which are responsible for direct implementation within the states.
Funding through the NPHCDA Gateway consists of Programmatic fund for Decentralized Facility Funding (35%), which is made up of funding for essential drugs, vaccines, and consumables (20%) and maintenance of primary healthcare facilities, equipment, and transport(15%). The remaining 10% for the NPHCDA Gateway is for Human Resource for PHC interventions consisting of 5% for midwives’ and 5% for Community Health Influencers and Promoters Agents (CHIPS).
The NPHCDA Gateway is to ensure operational funding to strengthen the delivery of primary careservices across the entire country, prioritizing rural public primary health care (PHC)facilities, to target poor households and populations in the lowest wealth bracket, a critical step towards attaining the SDG and Universal Health Coverage (UHC).
As a prerequisite for states to be on-boarded and benefit from the BHCPF, the following criteria need to be fulfilled:
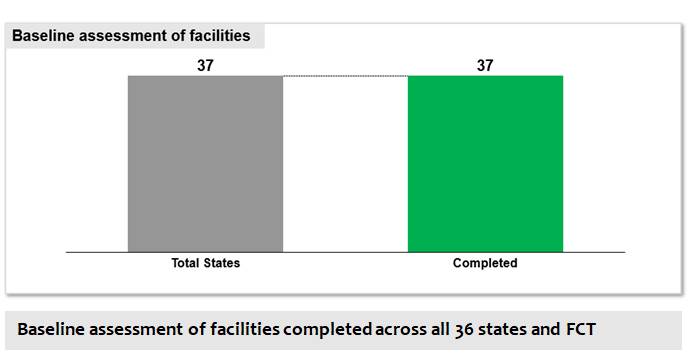
- Baseline assessment of BHCPF health facilities
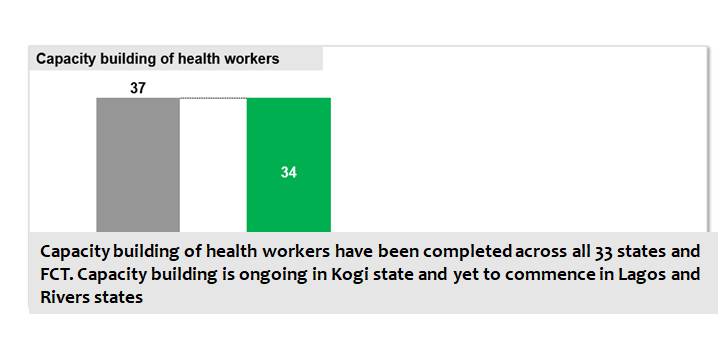
- Capacity building of health workers in the state to ensure health workers can effectively carry out their functions.
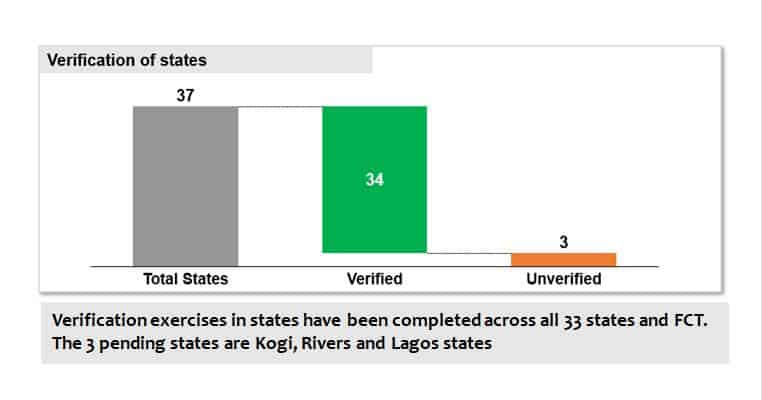
- Verification of all levels of implementation at the state
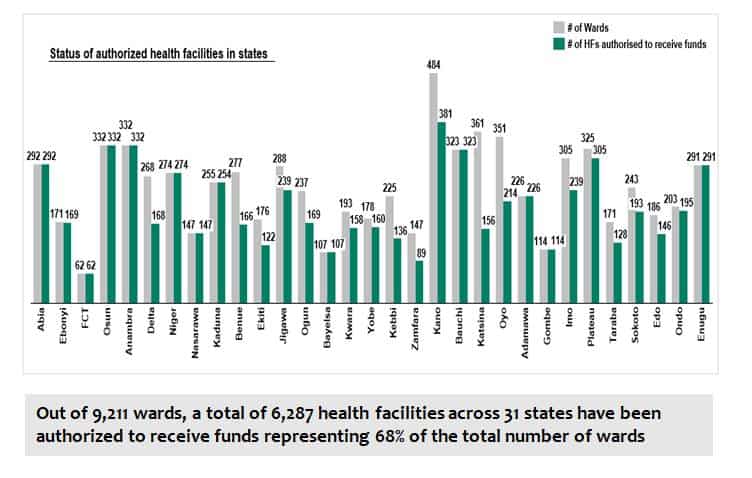
- Authorization for disbursement of DFF to eligible PHCs.
With the DFF, the PHCs are able to meet their operational cost, purchase essential medicines, and provide services based on the BMPHS, with expectation of reimbursement from the NHIS Gateway.
NPHCDA GATEWAY IMPLEMENTATION STATUS AS AT 31ST OCTOBER 2021
Documents and Reports
- BHCPF Guideline and NPHCDA Gateway Handbook
Bulletin and Publications
- NPHCDA Gateway Quarterly Information Bulletin
- Publications related to the NPHCDA Gateway
AIM OF BHCPF
OBJECTIVES OF BHCPF
- To achieve at least 1 (one) fully functional public or private primary health care (PHC) facility in each political ward; at least 30% of all wards over the next 3 years, 70% within 5 years, and 100% within 7 years.
- To achieve at least 3 (three) fully functional public or private secondary health care facilities, benefitting from the BHCPF in each state; at least 50% of all states over the next 3 years, and 100% within 5 years.
- To establish effective emergency medical response services in 36 states and the Federal Capital Territory (FCT) in 5 years, including a national ambulance service.
- To reduce out-of-pocket expenditure by 30% in 5 years and increase financial risk protection through health insurance.
- To increase life expectancy to at least 60 years over the next 10 years.
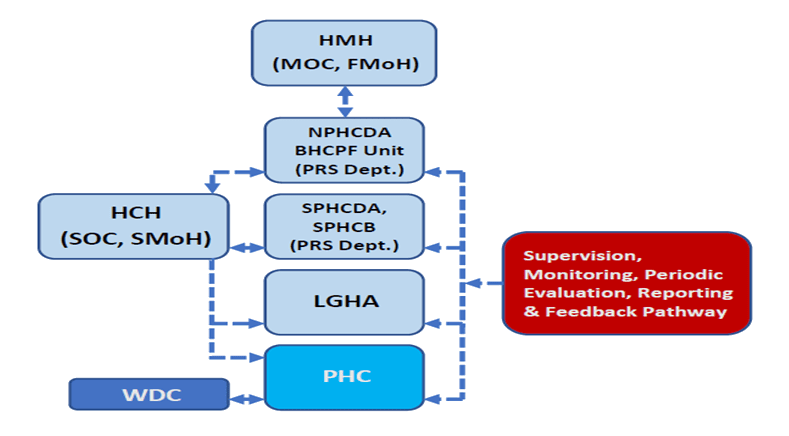
ORGANOGRAM OF THE GOVERNANCE STRUCTURE OF THE BHCPF
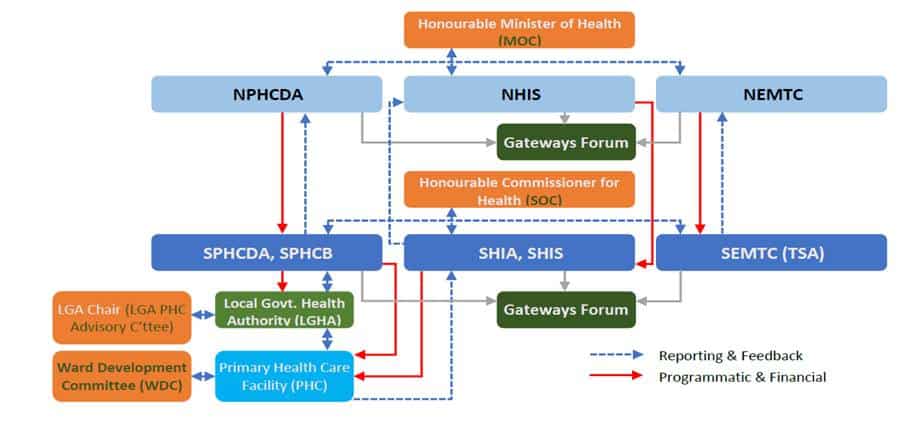
Ministerial Oversight Committee (MOC): This is chaired by the Honorable Minister of Health with membership across relevant agencies and stakeholders in the country.
State Oversight Committee (SOC): This is chaired by the Honorable Commissioner for Health with membership across relevant agencies and stakeholders in the state.
CORE FUNCTION OF STAKEHOLDERS
State Primary Health Care Boards (SPHCBs): Provide state level capacity and implementation of the NPHCDA Gateway activities with support from and in collaboration with the NPHCDA as well as provide direct technical support for BHCPF implementation at state, local government, and community levels.
Local Government Health Authority (LGHA): Work with the SPHCB for the implementation of the NPHCDA Gateway as well as provide direct technical support for implementation of BHCPF activities in PHCs such as in conducting routine supportive supervision and monitoring of PHCs in the LGAs
Ward Development Committee (WDC): Serve as members of the PHC Facility Quality Improvement Committee and collaborate with the PHC facility leadership in identification of and planning for health and social needs of the ward.
Primary Health Care Centers (PHCs): Provide quality services included in the BMPHS, to enrolled community members.
NPHCDA GATEWAY IMPLEMENTATION STATUS AS AT 31ST OCTOBER 2021
Implementation of the NPHCDA Gateway commenced in May 2019. Implementation required states to be onboarded after meeting the prerequisite criteria. So far, a total of 31 states have been onboarded into the program and a total of 6,287 health facilities across these 31 states have been cleared to receive DFF. Key highlights of implementation are outlined below: